The ONE organ responsible for high blood pressure.
Just the Essentials of Essential Hypertension
ACE inhibitors, used alone or in combination with diuretics and digoxin, both prevent congestive heart failure and reduce morbid and mortal events in patients with established failure and therefore are recommended as first-line agents for treating hypertensive patients with this condition.
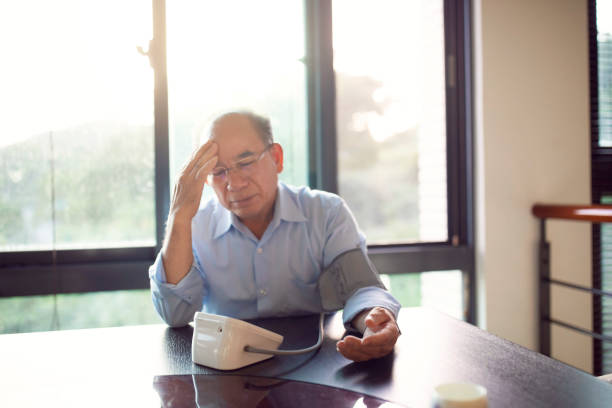
If essential hypertension is not diagnosed, the condition has the potential to worsen and create heart or kidney problems. Sometimes, people with essential hypertension may experience headaches, dizziness and blurred vision, but these symptoms are unlikely to occur until blood pressure reaches very high levels.
What is essential hypertension?
Essential hypertension is high blood pressure that doesn’t have a known secondary cause. It’s also referred to as primary hypertension. Blood pressure is the force of blood against your artery walls as your heart pumps blood through your body. Hypertension occurs when the force of blood is stronger than it should be normally. Most cases of high blood pressure are classified as essential hypertension. The other kind of hypertension is secondary hypertension. Secondary hypertension is high blood pressure that has an identifiable cause, such as kidney disease.What are the risk factors associated with essential hypertension?
Genetic factors are thought to play a role in essential hypertension. The following factors may increase your risk of developing essential hypertension:- diet
- stress
- minimal physical activity
- being overweight
What are the symptoms of essential hypertension?
Most people won’t notice any symptoms of essential hypertension. They usually discover that their blood pressure is high during a regular medical checkup. Essential hypertension can begin at any age. It most often occurs first during middle age.How will I know if I have essential hypertension?
Blood pressure checks are the best way to screen for the condition. It’s important to understand how to take your blood pressure and read the results. Blood pressure readings have two numbers, usually written this way: 120/80. The first number is your systolic pressure. Systolic pressure measures the force of blood against your artery walls as your heart pumps blood to the rest of your body. The second number measures your diastolic pressure. Diastolic pressure measures the force of your blood against your artery walls between heartbeats, as the heart muscle relaxes. Learn more about systolic and diastolic pressure. Your blood pressure readings can fluctuate up or down throughout the day. They change after exercise, during rest, when you’re in pain, and even when you’re stressed out or angry. Occasional high blood pressure readings don’t necessarily mean you have hypertension. You won’t receive a diagnosis of hypertension unless you have high blood pressure readings at least two to three different times.Normal blood pressure vs. abnormal blood pressure
Normal blood pressure is less than 120/80 millimeters of mercury (mmHg). Elevated blood pressure is higher than normal blood pressure, but not quite high enough to be hypertension. Elevated blood pressure is:- systolic pressure of 120 to 129 mmHg
- diastolic pressure less than 80 mmHg
- systolic pressure of 130 to 139 mmHg, or
- diastolic pressure of 80 to 89 mmHg
- systolic pressure higher than 140 mmHg, or
- diastolic pressure higher than 90 mmHg
How is essential hypertension diagnosed?
Your doctor will test your blood pressure using a blood pressure monitor. If your blood pressure is high, they may want you to check your blood pressure at home during regular intervals. Your doctor will teach you how to use a blood pressure monitor if they ask you to measure your blood pressure at home. You’ll record these readings and discuss them with your doctor at a later date. The severity of your high blood pressure is determined by the average of your blood pressure readings taken at different times. Your doctor may perform a physical exam to check for signs of heart disease. This exam may include looking at your eyes and listening to your heart, lungs, and blood flow in your neck. Small blood vessels in the back of your eye can indicate damage from high blood pressure. Damage here indicates similar damage elsewhere. Your doctor may also order the following tests to detect heart and kidney problems:- Cholesterol test. Also called a lipid profile, this will test your blood for your cholesterol levels.
- Echocardiogram. This test uses sound waves to make a picture of your heart.
- Electrocardiogram (EKG or ECG). An EKG records the electrical activity of your heart.
- Kidney and other organ function tests. These can include blood tests, urine tests, or ultrasounds to check how your kidneys and other organs are functioning.
How is essential hypertension treated?
There’s no cure for essential hypertension, but there are treatments. Lifestyle changes If you have elevated blood pressure or hypertension, your doctor will recommend lifestyle changes to lower your blood pressure. Lifestyle changes your doctor may recommend include the following:- Exercise at least 30 minutes a day.
- Lose weight if you’re overweight.
- Quit smoking.
- Limit your alcohol intake to no more than one drink a day if you’re a woman and two drinks a day if you’re a man.
- Reduce your stress levels.
- Eat a low-sodium, heart-healthy diet that’s rich in potassium and fiber.
- If you have kidney problems, don’t increase your potassium intake without your doctor’s permission.
- beta-blockers, such as metoprolol (Lopressor)
- calcium channel blockers, such as amlodipine (Norvasc)
- diuretics, such as hydrochlorothiazide/HCTZ (Microzide)
- angiotensin-converting enzyme (ACE) inhibitors, such as captopril (Capoten)
- angiotensin II receptor blockers (ARBs), such as losartan (Cozaar)
- renin inhibitors, such as aliskiren (Tekturna)
What are the complications associated with essential hypertension?
The higher your blood pressure is, the harder your heart has to work. A stronger force of blood can damage your organs, blood vessels, and heart muscle. This can eventually cause reduced blood flow through your body, leading to:- heart failure
- heart attack
- atherosclerosis, or hardening of the arteries from cholesterol buildup (can lead to a heart attack)
- stroke
- eye damage
- kidney damage
- nerve damage