The #1 Rated Blood Sugar Formula
The Impact of Venous Hypertension on Circulatory Health: What You Need to Know
Getting to Know Venous Hypertension
What is Venous Hypertension?
Venous hypertension might not grab as many headlines as its arterial counterpart, but it's an important condition to understand. It happens when blood pressure in the veins gets too high, usually because the valves within the veins aren't working properly. This valve failure leads to blood pooling and extra pressure. Unlike arterial hypertension, which affects arteries, venous hypertension is all about the veins, bringing its own set of challenges and health issues.
Why Does Venous Hypertension Occur?
The reasons behind venous hypertension are quite varied. It often involves a mix of genetic factors, long periods of standing or sitting, being overweight, and not getting enough exercise. Things like aging, pregnancy, and having had deep vein thrombosis (DVT) can also increase the risk. Understanding how these factors play off each other is key to tackling the condition early.
Venous Hypertension vs. Other Hypertension Types
Both venous and arterial hypertension involve high pressure, but that's where the similarities end. Arterial hypertension affects arteries and can lead to heart problems, while venous hypertension affects veins and can cause varicose veins and chronic venous insufficiency. Knowing these differences is crucial for diagnosing and managing the condition correctly.
How Venous Hypertension Works
The Importance of Veins and Valves
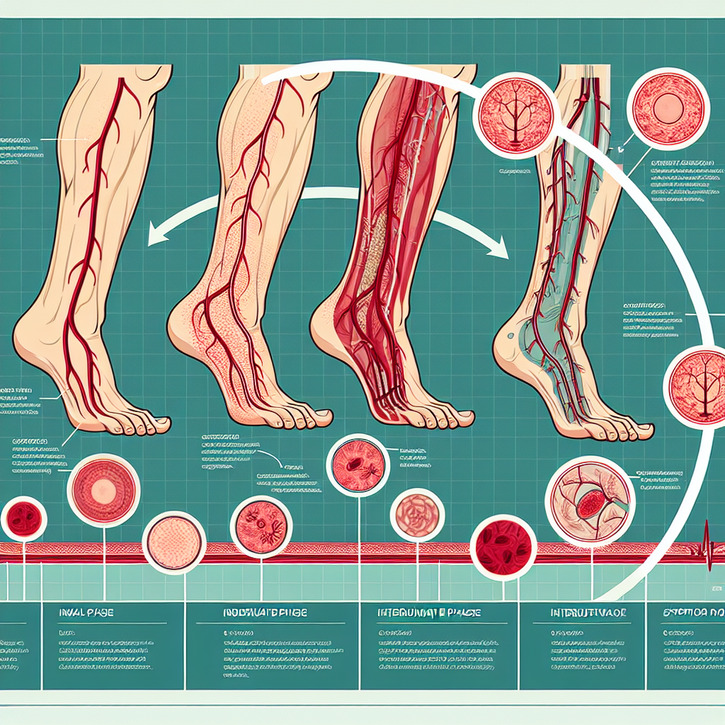
Veins are essential for returning deoxygenated blood to the heart, and they rely on valves to stop blood from flowing backward. When these valves fail in venous hypertension, blood pools and pressure increases, setting off a chain reaction of symptoms and complications.
Why Does Venous Pressure Rise?
Pressure increases in the veins mainly due to valve failure or some blockage in the veins. When valves don't do their job, gravity pulls blood back, raising pressure and causing veins to swell. Standing or sitting for too long can make this worse by hindering blood's natural return to the heart.
Effects on Circulation
Venous hypertension can throw the whole circulatory system off balance. It might lead to blood moving sluggishly, upping the risk of clots. Over time, this can cause skin changes, ulcers, and a higher risk of venous thromboembolism (VTE). Keeping venous pressure in check is vital for good circulatory health.
Spotting and Diagnosing Venous Hypertension
Signs to Look Out For
Symptoms of venous hypertension can be all over the place, but common ones include swollen legs, varicose veins, leg pain or heaviness, and skin changes like discoloration or ulcers. These might start off subtle but often worsen over time, impacting your daily life.
How is Venous Hypertension Diagnosed?
Diagnosing this condition usually involves a physical exam and some diagnostic tests. A Doppler ultrasound is a non-invasive way to check blood flow and valve function. Sometimes, venography is used for a detailed look at the veins. Catching the condition early is crucial to managing it effectively and avoiding complications.
Why Early Detection Matters
Spotting venous hypertension early can help prevent long-term problems and improve outcomes. Noticing symptoms early and getting medical advice can lead to interventions that slow the disease's progress and improve life quality. Regular check-ups and knowing your personal risk factors are key to early detection.
How Venous Hypertension Affects Your Circulation
Impact on Blood Flow
Venous hypertension can mess with blood flow, causing blood to pool in your legs. This limits oxygen and nutrients reaching tissues, leading to discomfort and possible damage. Over time, poor circulation can lead to chronic venous insufficiency and other circulatory issues.
Potential Complications
If left untreated, venous hypertension can lead to serious problems like skin changes, venous leg ulcers, and a higher risk of deep vein thrombosis (DVT). These not only harm physical health but can also have emotional and social impacts, highlighting the need for early treatment.
Long-term Health Effects
Chronic venous hypertension can result in ongoing issues like swelling, pain, and skin changes. If ignored, these can lead to more severe problems such as venous ulcers and infection risk.
Treatment and Management Strategies
Making Lifestyle Changes
Adjusting your lifestyle is a major part of managing venous hypertension. Regular exercise, lifting your legs, and keeping a healthy weight can ease symptoms. Home remedies like compression garments and leg elevation can also boost blood flow and lower vein pressure.
Medical Treatments
Treating venous hypertension medically might involve medications to improve blood flow and reduce pain, or procedures like sclerotherapy or endovenous laser treatment. These aim to enhance vein function and reduce symptoms, helping you live better.
When Surgery is Needed
For more serious cases, surgery might be on the table. Options like vein stripping or ligation can help by removing or closing off damaged veins to enhance blood flow. While surgery is usually for advanced cases, it can provide significant relief.
Prevention and Lifestyle Tips
Why Exercise Matters
Regular activity is key to preventing and managing venous hypertension. Exercise boosts blood flow, strengthens muscles supporting veins, and lessens pressure. Walking, swimming, and cycling are especially good for circulatory health.
Eating Right
A balanced diet supports vein health and lowers venous hypertension risk. Nutrients like fiber, flavonoids, and antioxidants improve circulation and reduce inflammation. Staying hydrated and watching salt intake can help prevent swelling and support overall health.
The Role of Compression Garments
Compression garments are an easy yet effective way to manage venous hypertension. They apply gentle pressure to legs, aiding blood flow and reducing swelling. They're particularly helpful for those who stand or sit a lot, offering support and symptom relief.
Navigating Life with Venous Hypertension
Finding Support and Coping
Living with venous hypertension can be tough, but finding strategies and support can make a big difference. Support groups, counseling, and stress management techniques can help manage the emotional and psychological aspects of the condition.
Keeping Track of Symptoms
Regularly monitoring symptoms and managing them proactively helps keep venous hypertension in check. Tracking symptom changes and staying in touch with healthcare providers ensures timely treatment adjustments.
When to See a Doctor
It's important to consult a healthcare professional if symptoms persist or worsen. Early intervention and expert guidance can help prevent complications and improve outcomes. Regular check-ups and open communication are essential for effective management.
Looking Ahead in Venous Hypertension Research
New Treatments on the Horizon
Research in venous hypertension is progressing, with new treatments and innovations on the way. Future developments, from new medications to less invasive procedures, hold promise for better treatment outcomes and quality of life improvements.
What's Trending in Research?
Current research focuses on understanding the genetic and molecular factors behind venous hypertension and exploring new treatment options. These efforts aim to deepen our understanding and pave the way for more effective interventions.
Improving Patient Outcomes
The future of managing venous hypertension looks bright, with the potential for better patient outcomes through ongoing research and innovation. Staying informed about the latest advances gives hope for more effective treatments and enhanced quality of life.

Maja Kowalczyk is a health enthusiast and has been interested in healthy and natural methods of regulating blood pressure for many years.